Winning the Battle Against Teeth Cavities: Causes, Symptoms, and Proven Treatments
Fact checked
By Lily Duffy, BDS, MRes, MPaed, NHS Leadership Fellow
Last Updated on November 2nd, 2023 / Published on August 9, 2023

Tooth cavities are not fun! Dealing with them can be distressing, so it’s important to understand what causes them and how to treat them.
Cavities, also known as dental caries or tooth decay, are among the most common diseases worldwide. According to the World Health Organization (WHO), dental decay affects more than 50% of school-aged children1 and at least 90% of adults.1
The impact of tooth decay can be severe, ranging from physical symptoms to a lack of self-confidence and dental phobia.
This article aims to empower you with knowledge about tooth decay and the importance of early detection and treatment so that you can make informed decisions about your oral health and adopt optimum preventative measures.
What Causes Teeth Cavities?
Cavities are a result of dental decay, also known as caries. Several factors increase the risk of cavity development and progression.
- Oral bacteria, notably Streptococcus mutans, are present in the mouth. These oral bacteria feed on carbohydrates (sugars), producing acid as a by-product.
- The acid then erodes tooth enamel through a process called demineralization, thereby weakening the tooth surface.2
- A diet high in sugary foods and beverages provides more carbohydrates for the oral bacteria to metabolize, increasing acid production and the likelihood of cavity formation.2
Are Some People’s Teeth More Prone to Cavities?
Some individuals are indeed at an increased risk of developing dental cavities. Some people inherit genes that make them more vulnerable to cavities, while others have lifestyles that increase cavity risks.
Genetic Predisposition to Tooth Decay
Some people inherit weaker tooth enamel.3 This makes the tooth more prone to cavity development. Some may also have genetic disorders that lead to tooth shape and size anomalies, making them more challenging to clean.
Environmental and Lifestyle Factors Can Increase Cavity Development
The following are some environmental and lifestyle factors that can make you more prone to developing cavities4:
- Diet: Frequent consumption of sugary or acidic foods and beverages creates the ideal environment for oral bacteria to thrive.

2. Oral Hygiene: Poor oral hygiene practices, such as inadequate brushing, increase the accumulation of plaque and bacteria.
3. Lack of Fluoride: Fluoride helps strengthen your tooth enamel. It also prevents bacteria from metabolizing sugars, reducing acid production. Therefore, a lack of fluoride does the opposite, making your teeth more prone to decay.
- Dry Mouth: Saliva lubricates your teeth and helps neutralize bacterial acids. Certain medications and medical conditions can cause dry mouth (xerostomia), reducing saliva flow and compromising the natural defense.

Preventing tooth decay
Although tooth decay is prevalent worldwide, more than 95% of this condition is preventable.
Correct oral hygiene and dietary practices can significantly reduce the risk of dental decay.5
Here are some things you can do to prevent tooth decay:
- Good Oral Hygiene: Brush your teeth at least twice daily with fluoride toothpaste. This is fundamental to oral hygiene. It’s important to brush all surfaces of your teeth and tongue to remove bacteria gently. Floss daily! This helps remove plaque and debris between teeth. Mouthwash can be valuable to your oral hygiene routine but should not replace brushing and flossing.

- Balanced Diet: Eat a balanced diet daily. A balanced diet that supports oral health limits sugary and acidic foods and drinks and includes plenty of protein and vegetables, with minimal snacking between meals.

- Fluoride Use: Use fluoride toothpaste and, if your dentist recommends, consider fluoride treatments or mouth rinses.

- Dental Sealants: Dental sealants are thin, protective coatings applied to the chewing surfaces of back teeth to prevent cavities from forming in the grooves and pits.

- Regular Dental Check-ups: Visit your dentist regularly for check-ups and cleanings to identify and address dental issues promptly.

- Saliva Substitutes: Your dentist may recommend saliva substitutes or other strategies to combat dry mouth symptoms if you have a dry mouth.
Can Cavities Cause Health Problems Beyond the Mouth?
Yes, cavities can cause problems in other areas beyond your mouth. The bacteria in your mouth metabolize sugars and carbohydrates. The primary by-product of this metabolic process is acid.
When bacteria produce this acid, it causes demineralization of tooth enamel, leading to decay and cavities. The decay then promotes further bacterial accumulation, increasing the bacterial load.
Evidence suggests that this bacterial load can cause other systemic health issues. However, scientists do not fully understand this link and more research is needed.
There is also evidence to show poor oral health has a significant impact on quality of life. The following are links between oral health and overall well-being6:
- Inflammation: The mouth is home to numerous good and harmful bacteria. When oral health is compromised, harmful bacteria can thrive, leading to inflammation.
- Nutrition: Painful or damaged teeth can make it difficult to chew certain foods, leading to a limited diet that may lack essential nutrients.
- Psychological effects: Oral health issues can lead to self-consciousness and reduced self-esteem.
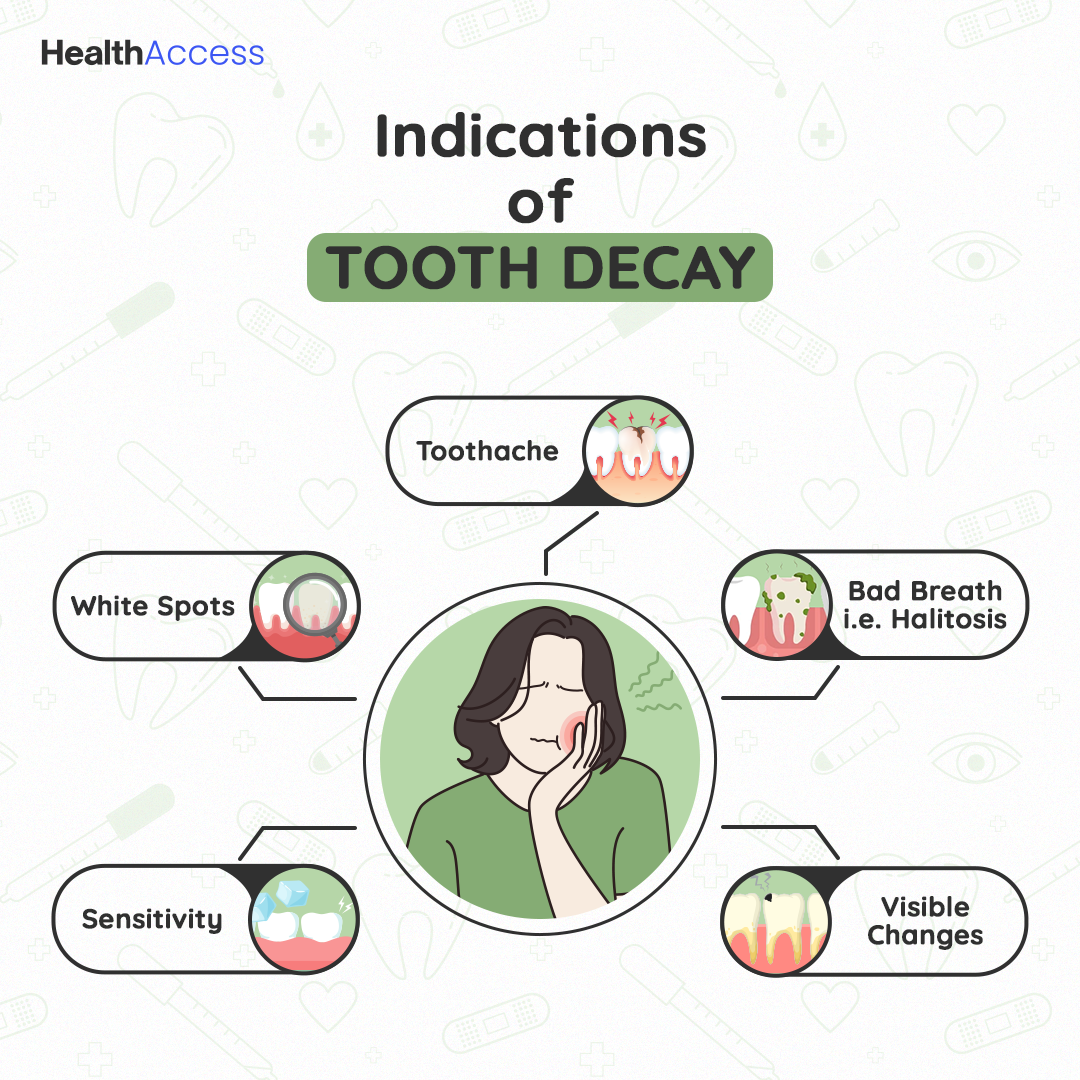
Teeth Cavities Symptoms: Identifying the Early Signs
Early Stages of Tooth Decay: Initial Indications
Identifying the early signs of tooth decay is crucial for timely intervention and preventing more severe dental problems.7
- Toothache: You may experience mild, intermittent pain or discomfort in the affected tooth. The pain can be dull or sharp and may worsen with exposure to certain stimuli.

- White Spots: Chalky white spots on the surface of your teeth highlight where the enamel is starting to demineralize.

- Bad Breath (Halitosis): Bacteria contributing to tooth decay can produce foul-smelling odors in the mouth, leading to persistent bad breath.

- Sensitivity: You might feel discomfort or pain when eating or drinking something hot, cold, sweet, or acidic.

Advanced Cavity Symptoms
If tooth decay progresses without proper intervention, the cavities will become more advanced.8
- Increased Tooth Sensitivity and Pain: As the cavity progresses, the sensitivity of the affected tooth may intensify, and the pain may become more frequent and severe.
- Visible changes: The affected tooth may turn yellow, brown, or black as the decay spreads. The cavities may also become larger, making them visible to the naked eye.
- Pus or Abscess Formation: In severe cases, a dental abscess may develop, forming pus around the affected tooth.
Understanding Tooth Sensitivity and Pain as Cavity Symptoms
Sensitivity often occurs in the early stages of enamel demineralization.9 The loss of enamel exposes the underlying dentin, which contains tiny tubules that connect to the nerve endings in the tooth.
Exposing these tubules to stimuli like hot or cold, sweet, fluid movement within the tubules can trigger sensitivity. As the decay progresses, this fluid moves closer to the pulp, resulting in pain that may be more severe and persistent.
When Do Cavities Start to Hurt?
Tooth decay is a gradual process that progresses through the different stages10 below:
- Plaque buildup: Plaque is a sticky, colorless film comprising over 70% bacterial organisms, food particles, and saliva.
- Demineralization stage: As bacterial acids demineralize tooth enamel, they remove essential minerals such as calcium and phosphate, thus weakening the enamel structure.
- Enamel stage: The enamel continues to break down, getting closer to the soft dentin underneath. At this stage, the tooth structure is compromised, and a cavity starts to form.
- Dentin stage: Decay spreads rapidly through soft dentin, which is more porous and less resistant than enamel.
- Pulp stage: Decay will eventually reach the tooth pulp. The pulp contains blood vessels, nerves, and connective tissue. Therefore, it’s only when decay has evaded all of your dentin layer and reached the pulp (closer to the nerves) that it starts to hurt! As the decay progresses through the dentin and moves closer to the pulp, the risk of pain increases.9
Some individuals may experience mild discomfort or sensitivity even in the early stages of cavity development. In contrast, others may not feel pain until the decay becomes more advanced.
Teeth Cavities Treatment: Effective Strategies and Approaches
Many professional treatment options are available for cavity management. They include the following:
1. Dental Fillings: Materials and Techniques11

Dental fillings are one of the most common treatments for cavities. They involve removing the decayed portion of the tooth and filling the space with a suitable material to restore the tooth’s structure and function. The following are different materials for dental fillings:
- Amalgam: Made from a combination of metals (silver, tin, copper, and mercury). They are durable and less expensive but may be less aesthetically pleasing.
- Composite: Also known as tooth-colored or white fillings, they blend with the tooth’s natural color, making them more aesthetically appealing. They are suitable for visible areas of the mouth but may be less durable than amalgam fillings.
- Ceramic: Made of porcelain or other materials, these fillings are tooth-colored, more stain-resistant, and highly durable.
2. Root Canal Therapy for Advanced Cavities:

Root canal therapy involves removing an infected tooth pulp and disinfecting the pulp canal space.11 It is then sealed with a special filling material to prevent further bacterial ingress.
3. Non-Invasive Treatments for Early-Stage Cavities:

If your cavities are in the early stages, you’re in luck. Some non-invasive treatments are available, including the following:
- Fluoride Treatments: Fluoride strengthens tooth enamel and makes it more resistant to acid attacks from bacteria.12 It can also help remineralize a weakened enamel surface. You will find fluoride in toothpaste or applied professionally as a gel or varnish.
- Sealants for Preventing Cavities in Vulnerable Areas: Molars and premolars have deep pits and grooves prone to trapping food particles and bacteria. To prevent this, dental sealants can be applied to create a smooth surface over these grooves.13
Can Cavities Be Healed Naturally? Debunking Myths and Exploring Natural Remedies
Natural remedies may offer supplemental benefits but cannot heal or reverse tooth decay.
- Xylitol and Its Anti-Cavity Properties:
Xylitol is a naturally occurring sugar alcohol found in some fruits and vegetables. When bacteria consume xylitol, they cannot metabolize it, reducing acid production. Scientific studies have shown that using xylitol-containing gum can help reduce the risk of cavities.14
-
Oil Pulling and Its Impact on Oral Health:
Oil pulling is an ancient practice that involves swishing a natural oil in the mouth for several minutes before spitting it out. Advocates claim that oil pulling reduces harmful bacteria and plaque. However, there is no well-established evidence to confirm these claims.15
The Importance of Preventive Measures
Maintaining Good Oral Hygiene Practices
As discussed above, the best action to prevent tooth decay is adequate brushing and flossing to effectively remove the buildup of sugars in the mouth.16
Regular Dental Check-ups and Cleanings:
Routine dental cleanings and examinations are essential to prevent and diagnose dental issues.16
During your routine dental check-ups, you can expect the following:
- Early Detection of Issues: Regular dental check-ups allow dentists to identify dental issues at their initial stages, making them easier to treat.

- Professional Cleaning: Dental hygienists can remove stubborn deposits that are difficult to brush away with a toothbrush

- Addressing Habits: Some habits, such as teeth grinding (bruxism) or nail-biting, can damage dental health. Dentists can identify these habits during check-ups and provide advice on how to reduce these.

- Oral Cancer Screening: Dentists perform oral cancer screenings during regular check-ups. Early detection of oral cancer greatly improves the chances of successful treatment.

- Monitoring Dental Work: For those with dental restorations, such as fillings and crowns, regular check-ups allow the dentist to assess their condition and ensure they are functioning correctly.

Dental Health and Overall Well-being: The Holistic Connection
Research has shown that oral health can impact various bodily systems.17
- Inflammation: Poor oral health, such as gum disease (periodontitis), can lead to chronic inflammation in the mouth, thus releasing harmful bacteria and inflammatory mediators into the bloodstream.

- Infection: Severe untreated cavities can lead to dental abscesses, which are pockets of pus caused by bacterial infection. If the infection spreads, it can affect nearby tissues and even reach other body parts.

- Pregnancy Complications: Pregnant individuals with gum disease may be at a higher risk of certain complications, such as preterm birth and low birth weight.

- Arthritis: Some research has suggested a connection between gum disease and certain types of arthritis, such as rheumatoid arthritis.18
- Cardiovascular Health: The evidence suggesting gum disease may be associated with an increased risk of cardiovascular diseases is well established.19 Chronic inflammation in the mouth can lead to inflammation and arterial plaque buildup within the cardiovascular system, increasing the risk of heart disease and stroke.17

- Diabetes: Research has shown that uncontrolled diabetes can lead to oral health problems, and poor oral health can negatively impact diabetes management.20

Takeaway
In conclusion, you can reduce the risk of cavities and other dental issues by prioritizing preventive measures such as regular dental check-ups, adequate oral hygiene, and a balanced diet. Every individual deserves a cavity-free smile to be proud of!
References
- World Health Organisation. Sugars and dental caries. www.who.int. Published November 9, 2017.
- Clark M, Braun PA. Promotion of oral health and prevention of dental caries among children in primary care. JAMA. 2021;326(21):2139.
- Shaffer JR, Wang X, McNeil DW, Weyant RJ, Crout RJ, Marazita ML. Genetic Susceptibility to Dental Caries Differs between the Sexes: A Family-Based Study. Caries Research. 2015;49(2):133-140.
- Wang X, Willing M, Marazita ML, et al. Genetic and Environmental Factors Associated with Dental Caries in Children: The Iowa Fluoride Study. Caries Research. 2012;46(3):177-184.
- Ruff RR, Niederman R. Comparative effectiveness of treatments to prevent dental caries given to rural children in school-based settings: protocol for a cluster randomized controlled trial. BMJ Open. 2018;8(4).
- Sischo L, Broder HL. Oral health-related quality of life. Journal of Dental Research. 2011;90(11):1264-1270.
- Gomez J. Detection and diagnosis of the early caries lesion. BMC Oral Health. 2015;15(S1).
- Rathee M. Dental caries. https://www.ncbi.nlm.nih.gov/books/NBK551699/. Published March 6, 2023.
- Renton T. Dental (Odontogenic) pain. Reviews in Pain. 2011;5(1):2-7.
- Featherstone JD. The caries balance: the basis for caries management by risk assessment. Oral Health & Preventive Dentistry. 2004 ;2 Suppl 1:259-264.
- Featherstone JDB, Crystal YO, Alston P, Chaffee BW, Doméjean S, Rechmann P, Zhan L, Ramos-Gomez F. Evidence-Based Caries Management for All Ages-Practical Guidelines. Front Oral Health. 2021 Apr 27;2:657518.
- Marinho VC, Higgins JP, Logan S, Sheiham A. Topical fluoride (toothpastes, mouthrinses, gels or varnishes) for preventing dental caries in children and adolescents. Cochrane Database Syst Rev. 2003;2003(4)
- Wright JT, Crall JJ, Fontana M, Gillette EJ, Nový BB, Dhar V, et al. Evidence-based clinical practice guideline for the use of pit-and-fissure sealants: a report of the American Dental Association and the American Academy of Pediatric Dentistry. J Am Dent Assoc. 2016;147(8):672-82.e12.
- Rethman MP, Beltrán-Aguilar ED, Billings RJ, Hujoel PP, Katz BP, Milgrom P, et al. Nonfluoride caries-preventive agents: executive summary of evidence-based clinical recommendations. J Am Dent Assoc. 2011;142(9):1065–71.
- Gbinigie O, Onakpoya I, Spencer E, McCall MacBain M, Heneghan C . Effect of oil pulling in promoting oro dental hygiene: A systematic review of randomized clinical trials. Complement Ther Med 2016; 26: 47–54.
- Public Health England, Department of Health and Social Care, NHS England, NHS Improvement. Delivering better oral health: an evidence-based toolkit for prevention. Chapter 2: Summary guidance tables for dental teams. Updated 21 September 2021.
- Sabharwal A, Stellrecht E, Scannapieco FA. Associations between dental caries and systemic diseases: a scoping review. BMC Oral Health. 2021 Sep 25;21(1):472.
- Mehdipour A, Masoumi M, Shajari P, et al. Oral health-related quality of life and dental caries in rheumatoid arthritis patients: a cross-sectional observational study. J Med Life. 2022;15(6):854-859.
- Kotronia E, Brown H, Papacosta AO, Lennon LT, Weyant RJ, Whincup PH, Wannamethee SG, Ramsay SE. Oral health and all-cause, cardiovascular disease, and respiratory mortality in older people in the UK and USA. Sci Rep. 2021 Aug 12;11(1):16452.
- Latti BR, Kalburge JV, Birajdar SB, Latti RG. Evaluation of relationship between dental caries, diabetes mellitus and oral microbiota in diabetics. J Oral Maxillofac Pathol. 2018;22(2):282.